Prostate Cancer
Prostate cancer is the second most common type of cancer in men, and the third leading cause of cancer death. The cancers develop when a group of abnormal cells within the gland are able to grow without constraint, forming a malignant tumour that can then escape and invade either into surrounding structures, the lymph nodes, or more distant organs such as skeletal bones.
By the age of 85, 1 in 7 men will be diagnosed. Fortunately, many of these tumours will be slow growing and can either be safely watched, or will be caught in time for safe & effective treatment. Dr Symons strongly advocates for a conservative path of management where possible, whilst at the same time recognizing that for some men upfront treatment is best, so as to utilise the ‘window of opportunity’ for a succesful cure.
Following your biopsy, Dr Symons will review your particular scenario, and arrange additional staging scans as might be required. This helps to confirm that the tumour is located within the prostate, and helps to guide the treatments that might be required to offer you the best balance between cancer cure, preservation of quality of life, and treatment intensity.
Dr Symons practices ‘best practice’ cancer care and is actively involved in several Multidisciplanary Cancer Meetings. These team meetings, held routinely at no cost to the patient, involve a group of cancer experts (pathologists, imaging experts, medical & radiation oncologists, and fellow cancer surgeons), and offer re-review of the biopsy material, any scans done to date, and allow for multiple “second-opinions”. This ensures that the treatment plan a patient has is not just based on the years of experience & knowledge of one individual, but a whole room full!
The diagnosis of prostate cancer is understandably a trying time for most men. It is usual for people to face a multitude of emotions, and have a multitude of questions.
Dr Symons and the Sydney Uro team are here to support you on this journey, and will be only too happy to provide a sympathetic ear or provide any extra attention that you might require. We understand that after receiving an unwanted diagnosis, navigating the healthcare system can become even more challenging.
Dr Symons and the team want to minimise any stress that you or your family might feel, and will work with you to help streamline any additional appointments or investigations that might be required.
What is PSA?
The prostate specific antigen, or PSA, is a protein made only in the prostate gland. It has a role in healthy male function, specifically as a mucolytic enzyme. It is NOT specific to prostate cancer, but rather acts as an essential part of human reproduction. When a man ejaculates, the PSA travels with the rest of the semen until it hits the female cervix, where it dissolves the mucous plug to allow sperm to swim through and reach an egg.
- A guide for men undergoing prostate surgery: Resource booklet
- Continence Management following Prostate Surgery
- Prostate Biopsy – Video
- Prostate Cancer Resources – Healthy Male
- Cancer Council
- Prostate Cancer Foundation of Australia
- Urological Society of Australia and New Zealand
Prostate Cancer Diagnosis
The Cancer Diagnosis (Moving from Uncertainty to Clarity)
(The Process of Design Squiggle by Damien Newman, thedesignsquiggle.com)
Following a prostate biopsy, in your consultations with Dr Symons there are a series of key pieces of information that Dr Symons will gather for you to assist in the management of your cancer.
Grade – how aggressive is the cancer?
Stage – how far has the cancer spread?
Once this information is gathered, Dr Symons will be able to further outline the treatment options, particularly as they relate to your unique cancer situation, and arrange the treatment plan that best suits YOU.
Transperineal Prostate Biopsy (TPB)
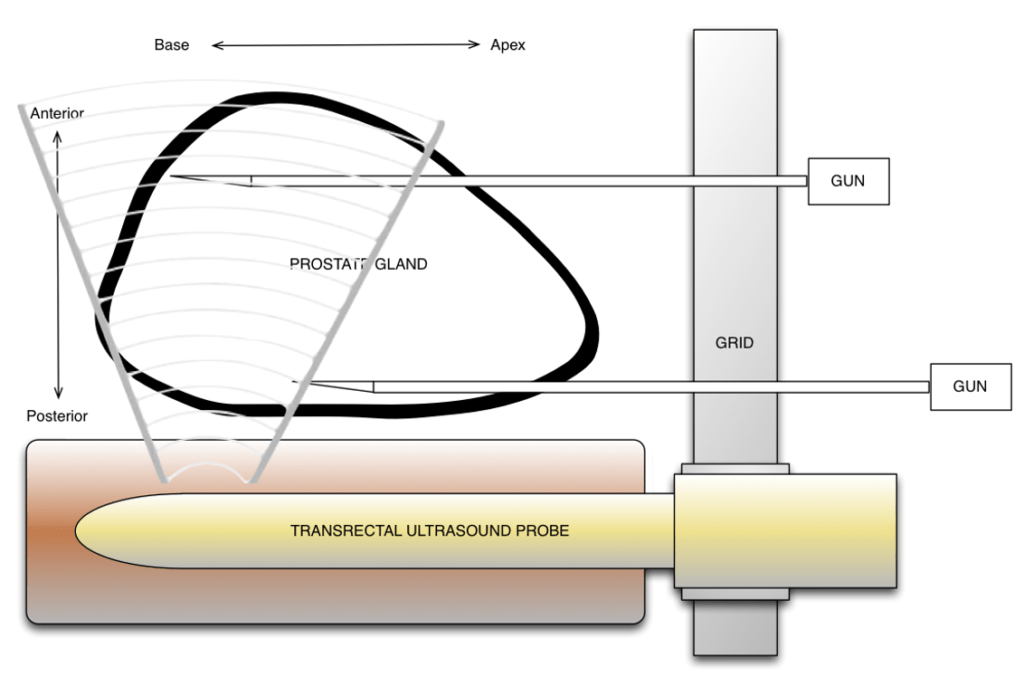
A safe and accurate biopsy technique is essential for the management of prostate cancer.
Patients are selected for biopsy based on a complex algorithm of their PSA and kinetics, examination findings, age and comorbidities, and individual risk factors for cancer. These include family history, patient concern of cancer, MRI findings, or a prior diagnosis of prostate cancer for which the patient is on an active surveillance program.
Dr Symons has been at the forefront of prostate cancer diagnosis and management for almost a decade. In 2013, Dr Symons authored the world’s largest series of the then new and safer Transperineal Prostate Biopsy. At the time, TPB accounted for < 0.5% of all biopsies done in Australia, with the remainder done through the more traditional transrectal route. This older style of biopsy, risking faecal contamination with each needle passage, can unfortunately miss 20-30% of tumours.
In 2016, Dr Symons was honoured to be invited to write the inaugural textbook on Transperineal Prostate Biopsy, a technique which has since continued to grow in popularity around the world.
As one of the world’s pioneers in this technique, Dr Symons uniformly performs Transperineal Prostate Biopsy. The advantages include:
- Increased biopsy accuracy
- Increased prostate sampling
- Extremely low risk of infective complication
- Ability for Dr Symons to fuse your MRI or PSMA PET scan with real-time ultrasound at the time of the procedure to further increase biopsy accuracy
Transperineal Biopsy is routinely performed in a day surgery under anaesthetic.
You will not feel much discomfort following the procedure, though it is common to see some blood in the urine and ejaculate for a short time afterwards.
Some men may find that the prostate gland swells, giving a transient restriction to the urinary flow.

Over the past 10 years Dr Symons has studied the evolving surgical techniques, with the majority of his cancer operations now performed using the Da Vinci robotic device. This allows for a more minimally-invasive procedure to completely remove the prostate (radical prostatectomy). Compared to open surgery, it conveys all the benefits of laparoscopy such as decreased pain, earlier mobilisation and return to work, lower blood loss, and a reduced hospital stay. As per open surgery, it confers excellent local cancer control, and for many men can give an earlier return to continence.
Prostate Cancer Treatments
Prostate cancer can be cured when it is localised to the prostate. Depending upon patient and tumour factors, it can be cured with either radiotherapy, surgery or a combined (multimodality) approach.


